The Role of Genetics in Cancer Development and Treatment
What are genes?
Genes are the basic hereditary units passed down from parent to offspring. Genes contain instructions for making proteins, which control the development and functioning of cells.
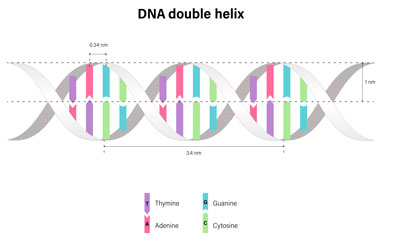 Genes are found in the DNA of every cell throughout the body. They control how the cell functions, including how quickly it grows, how often it divides, and how long it lives.
Genes are found in the DNA of every cell throughout the body. They control how the cell functions, including how quickly it grows, how often it divides, and how long it lives.
Protective genes aid in controlling cell growth and regulating the rate at which cells divide. They also assist in the repair of mismatched DNA. Mismatched DNA refers to errors that develop during the replication of DNA when a new cell is being formed.
When tumor suppressor genes are damaged or altered, their ability to protect or repair healthy cells is compromised, resulting in uncontrolled cell growth and the potential for cancerous tumors to form.
How do genes mutate?
What factors or exposures can cause a gene mutation?
- Biological factors include: increasing age, gender, inherited genetic defects, and skin type.
- Environmental causes include exposure to viruses such as Human Papillomavirus, Hepatitis B or Hepatitis C, and Human Immunodeficiency Virus (HIV). Other exposures include UV radiation (sunlight) and air pollution.
- Occupational exposures include chemicals, radioactive material, pesticides, and asbestos.
- Lifestyle factors include smoking, UV radiation (sun exposure or tanning beds), alcohol, obesity, diet (eating a diet high in processed foods, red meat, and saturated fats), and lack of exercise.
Want to learn more about tumor suppressor genes?
 There are several tumor suppressor genes. The most common tumor suppressor gene mutation is found in the p53 gene, which regulates cell division and initiates programmed cell death when necessary. Mutations in this gene can
lead to uncontrolled cell growth and the development of certain types of cancer, such as breast, ovarian, colorectal, lung, and pancreatic cancers.
There are several tumor suppressor genes. The most common tumor suppressor gene mutation is found in the p53 gene, which regulates cell division and initiates programmed cell death when necessary. Mutations in this gene can
lead to uncontrolled cell growth and the development of certain types of cancer, such as breast, ovarian, colorectal, lung, and pancreatic cancers.
Other tumor suppressor genes that have been linked to cancer when mutated include BRCA1 and BRCA2 (breast cancer), APC (colorectal cancer), PTEN (prostate cancer), RB1 (retinoblastoma), VHL (kidney cancer), and MSH2, MSH6, MLH1, and PMS2 collectively known as Lynch syndrome (hereditary non-polyposis colorectal cancer, endometrial cancer, stomach cancer, urinary tract cancers and more).
Remember, these genes typically protect us from developing cancer. It is not until they suffer a mutation that they lose this ability and can no longer effectively protect normal cell development.
Cancer genetics is a complex and rapidly evolving field of research. While researchers have made significant progress in understanding how specific genes can contribute to cancer, many cancers are not linked to a particular gene mutation. This suggests that cancer likely involves multiple gene mutations and interactions between genes and their microenvironment.
Is cancer inherited?
Cancer is a devastating disease that affects millions of people around the world. While it can affect anyone, some families seem to have an increased risk of specific cancer types. This phenomenon is known as family cancer syndrome, and it occurs when certain genetic mutations are passed down from one generation to the next. These mutations can increase the risk of developing certain types of cancer in members of the same family.
Family cancer syndromes or hereditary cancer syndromes are rare, but they are still important to be aware of. Knowing if your family has a history of any particular cancer type can help you and your physician take steps to reduce your risk, including monitoring for early detection. Early detection is critical when it comes to treating cancer, so being aware of any potential hereditary risks is essential for staying healthy.
I do not have cancer, but should I get genetic testing?
 When it comes to genetic testing for predicting cancer risk, the answer is not a simple yes or no. However, genetic testing can be incredibly beneficial in providing insight into an individual’s risk of developing cancer, but it should only be pursued under certain circumstances,
such as:
When it comes to genetic testing for predicting cancer risk, the answer is not a simple yes or no. However, genetic testing can be incredibly beneficial in providing insight into an individual’s risk of developing cancer, but it should only be pursued under certain circumstances,
such as:
- Those with a strong family history of cancer, especially if multiple relatives have been diagnosed with the same type of cancer, such as breast cancer, ovarian cancer, colon cancer, prostate cancer, and pancreatic cancer.
- Individuals diagnosed with one of the cancers associated with an inherited risk, such as breast and ovarian cancers.
- People belonging to certain racial or ethnic groups are predisposed to genetic mutations linked to particular cancer types, such as Ashkenazi Jews.
How genetics affect cancer treatment?
Today many tumors undergo genomic analysis once cancer has been discovered. The results of this type of genomic analysis play a significant role in cancer treatment, as it can help determine the best course of action for each individual patient. Genomic analysis can be used to identify mutations in genes that are associated with certain types of cancer, which can then be used to tailor treatments specifically for that patient. This is especially important regarding targeted therapies, such as immunotherapies and personalized medicines.
